Corneal cone – how does it manifest?
Meet the story of our patient
Julius, or Juluś as he was fondly called. He wasn’t exactly small. On his first visit to us, he was 21 years old, standing solidly over 190 centimeters tall, with the air of a determined young man. He came for an examination with his worried mother, who seemed visibly concerned. For the past few months, Juluś had been experiencing increasing eye itching and worsening vision, especially after sunset. He admitted to us that he loved cars and used to enjoy racing with his friends in go-karts, but now he avoided it. He had no idea that he was dealing with a corneal cone.
As the initial symptoms appeared, he felt less confident behind the wheel of his car, and he was already afraid to borrow his parents’ car. Driving at night was the worst – flashes, reflexes, uncertainty about the distance and speed of oncoming cars. He had obtained his driving license three years earlier on the first attempt, and at that time, all tests came out fine. Now he felt that something was wrong. He began to squint regularly to see better. And he kept rubbing his eyes. He also noticed a deterioration in his vision. And his mother, when they met, started saying the same thing she said years ago – “Juluś, hey… don’t frown like that.” Juluś had begun to develop keratoconus. This is a process during which the cornea undergoes deformation and weakening. Protrusions and deformations appear on its surface, causing the symptoms described by the patient.
Fortunately, Juluś was not born a generation earlier. The only thing he could have counted on then were general recommendations for eye care, regular check-ups, and glasses. Unfortunately, this would not have stopped the progression of the condition. By the time the condition reached a very serious state, it would have ended with a corneal transplant. However, nowadays we have many more options. We cannot and must not wait for the problem to reach a critical state. Only a healthy cornea enables proper vision. Therefore, at Blikpol, we conduct a qualification examination, select the method of corneal cone treatment, and proceed with the procedure. In our facility, we use several methods of corneal cone treatment, all of which are effective. Corneal cone treatment is currently very effective, but after the procedure, it is important to follow the doctor’s recommendations.

How to treat keratoconus?
Corneal cone (keratoconus) is a somewhat mysterious eye corneal disease, affecting roughly one in 1000-2000 people. The mystery arises from the fact that doctors don’t fully understand what causes it. We know that people who suffer from allergies, habitually rub their eyes, or have cases of keratoconus in the family are more susceptible. The occurrence of keratoconus is more common than one might think. In the initial stages of development, properly fitted soft or hard contact lenses may be sufficient. However, when the disease reaches an advanced stage, contact lenses are not enough – a procedure must be performed. Furthermore, in the early stages of the disease, the cone is most commonly located in the lower part of the cornea.

Cone treatment. How to treat corneal cone?
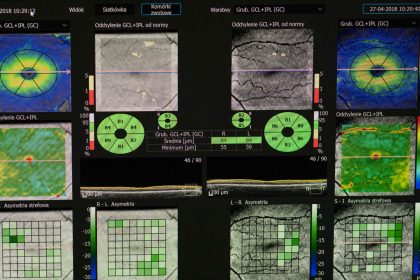
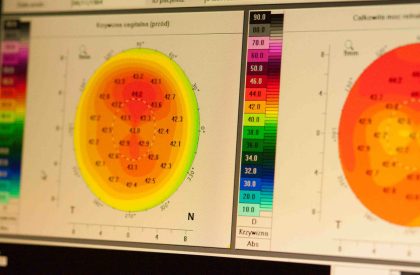
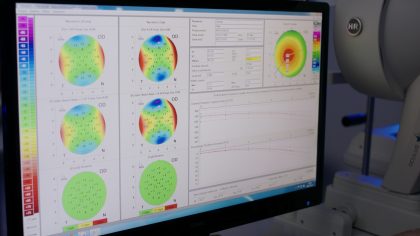
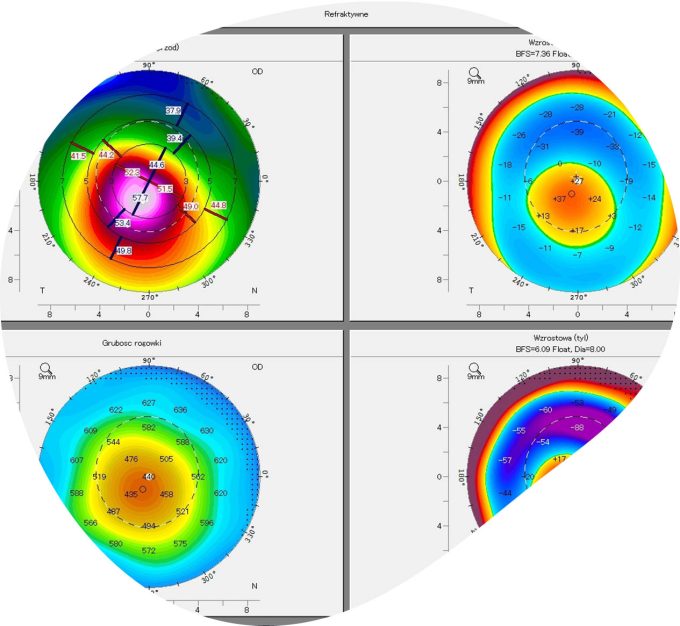
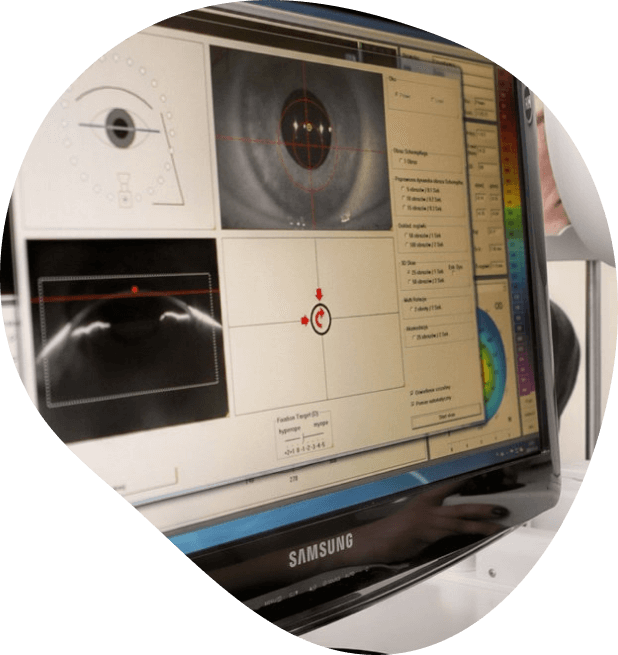
In patients, the cornea gradually becomes thinner over time, resulting in characteristic bulging. In the early stages of the disease, despite the best efforts of ophthalmologists, it is difficult to detect the condition in most standard-equipped offices. To confirm or rule out corneal disease, it is worth scheduling an appointment or taking someone with disturbing symptoms for the appropriate examination. During such an examination, corneal maps must be performed using high-specialized diagnostic equipment. Corneal examinations are also performed using a slit lamp. Such examinations are also conducted in our facility. If you are experiencing these symptoms, do not hesitate to see a specialist as soon as possible, who will perform the necessary examinations and implement appropriate treatment.
When is it worth having a corneal examination? If you or a close person are concerned about the following symptoms:
- Worsening vision, especially at night; increasing refractive error,
- Uneven deterioration of vision – first in one eye (increasing astigmatism and myopia, then in the other eye),
- Distorted or multiplied image in one eye,
- Prolonged light sensitivity,
- Itchy eyes, persistent urge to rub eyes,
- Sudden appearance of persistent blurred vision, eye pain for a prolonged period (although in most cases and most of the time the cone does not cause pain).
Forget about corneal cone
Corneal cone disease typically begins at a young age – in the teenage or early twenties, although it can also start in children. We understand that diagnosing a relatively rare condition can evoke fear, both in the patient and their parents. However, we reassure you – starting treatment early allows for halting the progression of the disease in a milder stage. When the first symptoms of corneal cone appear, it’s really not worth delaying examinations – they can only help and prevent the need for corneal transplant. Symptoms such as frequent eye rubbing should alert the patient and prompt them to make an appointment with an ophthalmologist in a professional ophthalmic office, where they will receive a diagnosis, learn about the causes of corneal cone formation, and if necessary, prepare for corneal cone correction surgery. It all depends on the stage of advancement of the corneal cone. In the initial phase, surgery may not be necessary. Untreated corneal cone can lead to the need for corneal cone transplantation. To avoid this, initial symptoms of the condition should not be ignored.
How is corneal cone treated?
At Blikpol, we employ the following methods to halt the progression of the disease and restore the cornea’s proper shape:
- Cross-linking using the Avedro KXL lamp,
- Insertion of intracorneal rings (Intacs),
- A dedicated combined method called Lasik Xtra – combining vision correction with cross-linking,
- Selection of specialized contact lenses (rigid gas permeable or soft and hybrid contact lenses).

These types of treatment methods halt the progression of corneal cone, improving visual acuity. It’s worth knowing that corneal cone typically does not develop simultaneously in both eyes. The disease most commonly develops in the teenage years and initially may be mistaken for allergies. Fortunately, more and more patients are learning about this condition and undergoing corneal cone treatment, which improves their vision without worsening refractive errors. Some patients may undergo combined procedures – CXL with laser corneal surface modeling, which restores the cornea to its normal shape. Femtosecond laser treatment can also be used.
It’s important to see a specialist as soon as the first symptoms appear. An ophthalmologist will conduct thorough examinations to confirm or exclude the diagnosis. Subsequently, appropriate treatment will be initiated, allowing the patient to return to full health. The total recovery period may last several weeks, but most patients return to their daily activities after just a few days. After the procedure, it’s important to follow the doctor’s instructions, which will help us quickly regain full health. We invite you to Blikpol. We use specialized equipment, and only qualified and experienced ophthalmologists work in our facility. By using our services, patients can be assured that they will be under the care of experienced ophthalmologists. In this case, it’s not worth delaying, as it’s a very risky action that can end in surgery.
How does a corneal cone manifest itself?
Corneal cone is a condition in which the cornea becomes thinner and begins to protrude outward, taking the shape of a cone. The corneal cone develops gradually, and one of the first signs is a sudden blurring of vision and progressive blurring of the image, which makes daily functioning difficult. Patients also often report multiple vision, the phenomenon of seeing several images of the same object, which is particularly noticeable at night. These symptoms are due to the abnormal shape of the cornea, which interferes with the proper focusing of light on the retina. In addition, there are changes in the lower eyelid area and discomfort due to the irregular shape of the cornea, which can affect the distribution of aqueous fluid in the eye and cause a feeling of dryness or irritation. The diagnosis of corneal cone requires specialized tests, such as measuring the curvature of the cornea and visiting a specialist.
Causes of corneal cone formation
Corneal cone is an eye disorder characterized by progressive bulging and shadowing of the cornea, leading to irregular astigmatism and consequent impairment of normal vision. The causes of corneal cone are not fully known, but genetics are believed to play a significant role in predisposition to the condition. In addition, corneal cone can be linked to allergic eye diseases that lead to frequent rubbing of the eyes, which in turn can contribute to increased pressure on the cornea and its deformation. Increasing astigmatism can be an early warning sign, suggesting a progressive corneal cone. Early diagnosis and monitoring of the corneal condition are key to stopping the progression of the disease and protecting against further vision deterioration. Modern medicine offers various treatments to stabilize the shape of the cornea and correct vision.
Early diagnosis of corneal cone
Early diagnosis of corneal cone is crucial for effective treatment and ensures that the progression of the disease is halted, which is essential for maintaining normal vision. Disturbing symptoms of corneal cone, such as rapidly increasing astigmatism, hazy vision or multiple vision, require prompt attention and consultation with an ophthalmologist. Allergic eye diseases that provoke frequent rubbing of the eyes can accelerate the progression of corneal cone, so it is important to pay attention to these aspects as well. Treatment of corneal cone in the early stages may include conservative methods, such as the use of rigid contact lenses, which help maintain the shape of the cornea and improve vision. In more advanced cases, surgical procedures are possible to strengthen the structure of the cornea and inhibit further deformation. If it has a corneal cone – treatment may include qualification for corneal cone surgery including cross linking.
Implantation of intracorneal ring segments INTACS®
In more advanced stages of keratoconus, we employ the procedure of implanting INTACS® rings. We use a femtosecond laser for this purpose. With its help, the doctor creates tunnels (corneal channels) in the eye, into which the rings are implanted. Unlike the older version of the procedure using manual dissectors, the procedure with the femtosecond laser is significantly more precise, safe, and fast.


In most cases, it does not require the use of sutures, which further shortens the healing time. The use of these technological solutions currently offers the greatest potential for effectively performing the procedure without the occurrence of both intraoperative and postoperative complications.
The entire procedure is performed under topical anesthesia, and after a short stay in the recovery room, you can return home. Both the implantation of INTACS and cross-linking therapy allow postponing the need for corneal transplantation for many years, and often indefinitely.
Specialized contact lenses
Such lenses are used to correct keratoconus at all stages of the disease’s development. They can be made from various materials and have different corrective properties.
The use of lenses allows for the correction of curvature – however, it primarily serves as assistance in combating the symptoms of keratoconus, rather than being the proper therapy to halt the progression of the cone. It is a supplementary solution to other methods.
All of these methods can also be combined if there are medical indications.
Each method can improve the patient’s vision; however, rings and cross-linking can postpone or completely eliminate the need for corneal transplantation for many years by significantly slowing down or halting the progression of the disease.
Important questions and answers
-
Corneal cone examination, also known as keratoconus, typically involves corneal topography. This is a detailed examination of the corneal surface using specialized equipment, which maps and measures the curvature and thickness of the cornea. Corneal topography helps the ophthalmologist identify characteristic changes associated with keratoconus, such as thinner and more conical areas. This examination is painless and usually takes a few minutes.
-
The cause of corneal cone is not fully understood. It is often associated with genetics, as it frequently occurs in several members of the same family. External factors such as intense eye rubbing, allergies, or wearing hard contact lenses may also influence the development of a cone. Additionally, keratoconus is more commonly diagnosed in individuals with certain conditions such as Down syndrome, Ehlers-Danlos syndrome, or asthma.
-
Corneal cone, also known as keratoconus, is a condition that can lead to worsening vision, but it is not directly dangerous to health. The main problem is the progressive deformation of the cornea, which leads to abnormal light refraction and consequently to vision disturbances. In advanced cases, if other treatment methods fail, a corneal transplant may be necessary. Regular monitoring of the corneal condition by an ophthalmologist is important.
-
Cross-linking procedure, also called CXL or collagen therapy, used in the treatment of keratoconus typically takes about 60-90 minutes. The process involves applying vitamin B2 (riboflavin) to the eye, followed by exposure to special UV light, which stimulates chemical bonds in the cornea, strengthening it and preventing further deformation. After the procedure, the patient needs to wear a protective contact lens, which helps to protect the eye and speed up healing.
-
Corneal cone (keratoconus) itself does not lead to complete blindness, but it can cause significant deterioration in visual acuity. In advanced cases of keratoconus, when the cornea becomes very thin and distorted, traditional methods of vision correction such as glasses or contact lenses may no longer be effective.
Price list
You may also be interested in:

Opinions

Safety

Make an appointment
Send us the form below if you want to schedule an appointment.
If you leave your phone number, we will call you back.